Hay fever, medically known as allergic rhinitis, is a widespread condition characterized by an allergic reaction to airborne allergens, primarily pollen.
Despite its name, hay fever does not cause a temperature but leads to irritating symptoms such as sneezing and itchy eyes.
This condition affects millions globally, especially during pollen season, when allergens are most abundant in the air.
Hay fever is an allergic response of the immune system to normally harmless particles classified as allergens.
When a person with hay fever inhales pollen or other triggers, their body produces histamine, causing inflammation in the nasal passages, eyes, and sinuses.

Symptoms of Hay Fever
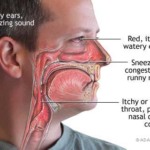
Common hay fever symptoms include sneezing, nasal congestion, a runny nose, itchy and watery eyes, and sinus pressure.
These nasal symptoms often resemble those of the common cold but tend to persist or recur seasonally.
Additional symptoms may include itchy throat and fatigue caused by disrupted sleep from nasal blockage.
People often confuse hay fever symptoms with symptoms of a cold, but hay fever typically does not cause fever or infectious symptoms.
Recognizing allergy symptoms early helps in effective management.
Causes of Hay Fever
Here are the 10 causes of hay fever:
Hay fever is primarily caused by an allergic reaction to airborne allergens, mainly pollen from grasses, trees, and weeds.
Environmental particles such as dust mite dander and animal dander can also trigger symptoms.
During the pollen season, the concentration of allergens in the air spikes. High pollen counts intensify allergic reactions.
Individuals predisposed to allergies have an overactive immune response where the body mistakenly treats pollen as harmful.
Asthma and hay fever are closely linked, as many people with hay fever also suffer from asthma symptoms, with both conditions involving airway inflammation triggered by allergens.
Key Stats of Hay Fever in US and Europe in 2025
Allergy & Allergic Rhinitis
“Allergic rhinitis” is the medical term for hay fever. It can be classified as seasonal allergic rhinitis, occurring during specific pollen-rich months, or perennial allergic rhinitis, which may persist year-round due to indoor allergens like dust mites or pet dander.
Both forms involve inflammation of the nasal passages and symptoms caused by a histamine-driven allergic reaction.

Allergy & Allergic Rhinitis: An In-depth Overview
“Allergic rhinitis” is the medical term used to describe what is commonly known as hay fever. It is a prevalent allergic condition affecting millions worldwide and occurs when the immune system mistakenly overreacts to otherwise harmless airborne substances called allergens.
The nasal passages become inflamed due to this immune response, leading to uncomfortable and often persistent symptoms triggered mainly by the release of histamine and other inflammatory mediators.
Different kinds of allergic rhinitis
Allergic rhinitis can be classified into two main forms based on timing and triggers: seasonal allergic rhinitis and perennial allergic rhinitis.
Seasonal allergic rhinitis occurs during specific pollen-rich months, typically spring, summer, or fall, when outdoor allergens like tree, grass, or weed pollen are abundant.
This form is commonly referred to as hay fever.
Perennial allergic rhinitis, on the other hand, can persist year-round and is often caused by indoor allergens such as dust mites, pet dander, cockroach droppings, or mold spores.
These allergens are present almost continuously in many homes and workplaces, leading to chronic inflammation of the nasal mucosa.
Immunological Mechanisms and Symptoms
The root of allergic rhinitis lies in an immunoglobulin E (IgE)-mediated hypersensitivity reaction.
Upon exposure to an allergen, the immune system triggers a cascade starting with mast cell degranulation and the release of histamine, leukotrienes, and prostaglandins.
Histamine plays a central role by causing sneezing, nasal itching, runny nose (rhinorrhea), and mucous gland stimulation. Other mediators promote blood vessel dilation and increased nasal congestion due to swelling and edema.
This allergic inflammatory response has both early and late phases.
The early phase, occurring within minutes of exposure, involves histamine release, while the late phase—occurring hours afterward—involves recruitment of eosinophils and other immune cells to the nasal mucosa, perpetuating inflammation and congestion.
Common symptoms of allergic rhinitis include sneezing, nasal congestion or stuffiness, a runny nose, nasal itching, postnasal drip, cough, and itchy, watery, red eyes, also known as allergic rhinoconjunctivitis when both nasal and ocular symptoms coexist.
These symptoms can significantly impair quality of life, affecting sleep, work, and social activities.

Triggers of Allergic Rhinitis
The most common triggers vary depending on geographic location and season:
- Tree pollens are prominent in early spring.
- Grass pollens dominate in late spring and summer.
- Weed pollens, such as ragweed, are common in the fall.
Indoor allergens such as dust mite feces, pet dander (from skin flakes, saliva, and urine), cockroach parts, and mold spores are typical causes for perennial rhinitis.
Brightly colored flower pollens rarely cause allergic rhinitis since they are too heavy to be carried by air.
The Relationship Between Allergic Rhinitis and Asthma
Allergic rhinitis frequently coexists with asthma, sharing common allergic pathways.
The “one airway hypothesis” suggests that upper and lower airways are parts of a single inflammatory airway disease.
Up to 40% of patients with allergic rhinitis may experience asthma symptoms like wheezing and shortness of breath triggered by similar allergens.
Diagnosis and Impact
Diagnosis usually relies on clinical history and symptom presentation, but allergy testing (skin prick or specific IgE blood tests) helps identify offending allergens, guiding management.
Severity varies from mild cases to moderate/severe forms where symptoms disrupt sleep and daily activities.
Allergic rhinitis is more than a nuisance; it can impair concentration, cause fatigue, and reduce productivity. Untreated, it may lead to recurrent sinus infections or exacerbate asthma.
Current Treatment Strategies
Treatment focuses on symptom relief and allergen avoidance:
- Antihistamines block histamine receptors, relieving sneezing and itching.
- Intranasal corticosteroids reduce mucosal inflammation and congestion.
- Decongestants provide short-term relief of nasal blockage.
- Nasal irrigation helps clear allergens and mucus.
For persistent symptoms unresponsive to medications, immunotherapy (allergy shots or sublingual tablets) offers a way to modify the immune response, often providing long-term benefits.
Pollen & Pollen Counts
Pollen is the primary allergen causing hay fever.
Plants release pollen grains to reproduce, and these microscopic particles spread via wind.
Monitoring pollen counts helps predict peak allergy times, enabling individuals to take preventive measures.
Higher pollen counts correlate strongly with increased severity of hay fever symptoms.
Asthma and Allergic Reaction
Many with hay fever also experience asthma symptoms triggered by similar allergens, creating what’s called an allergic airway disease continuum.
Managing both conditions requires coordinated care with allergy medications and avoiding allergens wherever possible. Untreated hay fever can worsen asthma control.
Symptoms and Causes
The core of hay fever’s symptoms is the body’s allergic response, which releases histamine, causing inflammation in the nose, eyes, and throat. Frequent triggers besides pollen include dust mites, dander, and mold.
The symptoms range from mild sneezing and itchy eyes to severe ones, like intense nasal congestion and sinus pain.
Combining these treatments improves symptom control and quality of life.
How to Reduce Symptoms of Hay Fever: 12 Effective Remedies
Managing hay fever symptoms effectively can significantly improve quality of life during allergy season. Here are 12 remedies grouped into allopathy, homeopathy, Ayurveda, and Yunani systems to provide a comprehensive approach.
Allopathy Remedies
- Antihistamines: Medications like cetirizine, loratadine, and fexofenadine block histamine effects, relieving sneezing, itching, and watery eyes.
- Nasal sprays: Use of steroid nasal sprays or decongestant nasal sprays reduces nasal inflammation and congestion.
- Eye drops: Antihistamine or lubricating eye drops soothe itchy, watery eyes.
- Nasal irrigation: Saline nasal washes or neti pots help clear allergens and mucus from nasal passages.
Homeopathy Remedies
- Apis Mellifica: Used for stinging nasal congestion, improved by cold air.
- Euphrasia: Helps with watery, swollen eyes and acrid tears accompanying hay fever.
- Ferrum phosphoricum is effective in the early stages of inflammation to slow symptoms like burning eyes and runny noses.
- Galphimia Glauca: Relieves spasmodic sneezing typical of hay fever.
Ayurvedic Remedies
- Haridrakhand: Herbal mix containing turmeric, known for anti-inflammatory effects.
- Nasya therapy: Application of medicated oils like Anu Tailam in nostrils to protect and soothe mucosa.
- Chyavana Prasham: Immunity-boosting herbal jam rich in vitamin C and antioxidants.
- Trikatu: A combination of black pepper, long pepper, and ginger used to reduce mucus and improve respiratory health.
Yunani Remedies
- Rudanti: An herbal formulation to reduce inflammation and mucus buildup.
- Jawafa: Traditionally used for calming allergic respiratory symptoms.
- Tukhm-e-Khyar Shambar: Cucumber seed preparation that cools and soothes the mucous membranes.
- Khamira Abresham Hakim Arshad Wala: A herbal compound for strengthening immunity and relieving respiratory allergies.
Combining these remedies under expert guidance can reduce hay fever symptoms effectively and improve overall well-being during allergy season.
Prevent Hay Fever
Preventative measures include:
- Allergy shots (immunotherapy) to gradually desensitize the immune system to allergens.
- Avoiding outdoor exposure on high pollen count days.
- Keeping windows closed and using air purifiers to reduce exposure to allergens in the air.
- Regular cleaning to minimize indoor allergens like dust and dander.
The right combination of allergy medicines, lifestyle modifications, and sometimes medical treatments helps prevent hay fever flare-ups effectively.
Understanding hay fever fully—its symptoms, causes, and treatments—empowers you to manage this common allergic condition confidently and keep symptoms under control throughout the challenging allergy season.
The condition affects 20% of adults in the UK and seems to be becoming more common in children.
About Hay Fever
If you’re allergic to pollen from grasses, weeds, or trees or molds carried in the air during the spring and summer, it means that you’re prone to hay fever.
These plants and molds produce allergens—substances that can cause an allergic reaction.
When your body’s immune system reacts to an allergen, for example, pollen, an allergic reaction happens because it mistakes it for a kind of viral invader.
The result of your immune system overreacting to pollen allergens leads to hay fever, which is airborne during spring and summer and which is less harmful to most people.
The tendency to develop hay fever (allergic rhinitis), food allergy, and eczema, which are related allergic conditions, seems to run in families.
This is called atopy. This means antibodies are produced in response to allergens in allergic people, while they’re not in non-allergic people.
Symptoms of Hay Fever
One can have one or more of the following as a range of symptoms. These include
- Sneezing
- A blocked or runny nose (rhinitis)
- Itchy nose, mouth, eyes, throat, skin, or any area
- Headaches
- Problems with smell
- Tearing eyes
- Sinus pressure and facial pain
- Swollen, blue-colored skin under the eyes (allergic shiners)
Symptoms that sometimes develop later include:
- Stuffy nose (nasal congestion)
- Coughing
- Clogged ears and decreased sense of smell
- Sore throat
- Dark circles under the eyes
- Puffiness under the eyes
- Fatigue and irritability
- Memory problems and slowed thinking
- Trouble Sleeping
- Postnasal drip
Other common physical symptoms (part of late-phase symptoms) include a decreased sense of smell or taste, plugged ears, sinus headache, postnasal drip, or some combination.

An allergic reaction can cause symptoms from harmless substances. These include dust, pet hair, and pollen. It can also trigger symptoms from harmful agents. These harmful agents include bacteria, viruses, and toxins.
This may lead to a runny nose, congestion, and throat irritation.
The activated immune system generates antibodies, leading to the release of histamines into the bloodstream.
This process results in symptoms such as itching, swelling of the affected tissues, increased mucus production, hives, rashes, and other related manifestations.
The manifestation of symptoms can differ significantly in intensity among individuals.
Comprehensive Guide to Hay Fever Relief and Management
Understanding the intricate details of hay fever symptoms, causes, and effective remedies is crucial for anyone suffering from allergic rhinitis.
Hay fever symptoms can manifest in various ways, from mild to severe, affecting individuals differently based on their allergic sensitivity and environmental exposure.
The key to successful hay fever relief lies in identifying your specific triggers—whether that’s seasonal pollen, dust mites, or animal dander—and implementing targeted strategies.
Modern hay fever treatment options range from over-the-counter antihistamines to prescription medications like intranasal corticosteroids, offering multiple pathways to manage symptoms effectively.
For those seeking long-term solutions, allergen immunotherapy and sublingual tablets can help modify your immune response, providing lasting hay fever relief.
Rhinorrhea and nasal congestion are common complications that can severely impact sleep quality and daily functioning, making proper treatment essential.
Understanding the distinction between seasonal allergic rhinitis and perennial allergic rhinitis helps in choosing the most appropriate management strategy for your specific situation.
Advanced Hay Fever Symptoms and Early Detection
Detecting allergic symptoms early can make a significant difference in managing your hay fever effectively throughout the season.
Watery eyes are one of the most recognizable signs of an allergic reaction, often accompanied by intense itching that makes it difficult to concentrate.
Postnasal drip, while seemingly minor, can lead to persistent coughing and throat irritation that disrupts daily activities and sleep patterns.
Many individuals experience allergic shiners—dark circles and puffiness under the eyes—which indicate chronic allergic inflammation.
Severe hay fever can impact cognitive function, with research showing that untreated allergy symptoms may impair concentration and memory.
Early intervention with antihistamines or intranasal corticosteroid sprays can prevent symptoms from escalating and becoming more difficult to control.
For those with persistent hay fever symptoms lasting more than a few weeks, consulting with an allergist for proper diagnosis is essential.
Long-Term Solutions for Severe Hay Fever and Chronic Allergy Management
For individuals dealing with persistent, moderate to severe hay fever that impacts their quality of life, exploring advanced treatment options becomes necessary.
Allergy shots, also known as subcutaneous immunotherapy, involve regular injections that gradually increase your exposure to specific allergens, helping your body build tolerance.
This proven hay fever relief method requires a multi-year commitment but offers long-lasting results that can persist even after treatment completion.
Sublingual immunotherapy tablets provide an alternative to injections, allowing patients to self-administer treatment at home while achieving similar immune system adaptation.
Maintaining consistent allergen avoidance strategies throughout peak pollen season remains essential, regardless of which treatment modality you choose.
Working closely with an allergy specialist ensures your hay fever treatment plan addresses your individual hay fever causes and symptom severity.
Regular monitoring of your response to treatment helps optimize your long-term hay fever relief strategy and prevents symptom flare-ups during critical times.
Combining multiple approaches—including environmental controls, medication, and immunotherapy—often yields the best outcomes for chronic hay fever management.